Imagine you’re sitting in a doctor’s office, waiting for your appointment, when you notice a poster on the wall about Horner Syndrome. The symptoms listed catch your attention, and you begin to wonder, which nerve root is affected in this condition? As you ponder this question, you realize that understanding the specific nerve root involved could hold the key to unraveling the mysteries of Horner Syndrome. But what is it about this particular nerve root that contributes to the development of this rare neurological disorder? In this article, we will embark on a journey to uncover the answer, exploring the intricate web of neural connections and shedding light on the fascinating world of Horner Syndrome.
Overview of Horner Syndrome
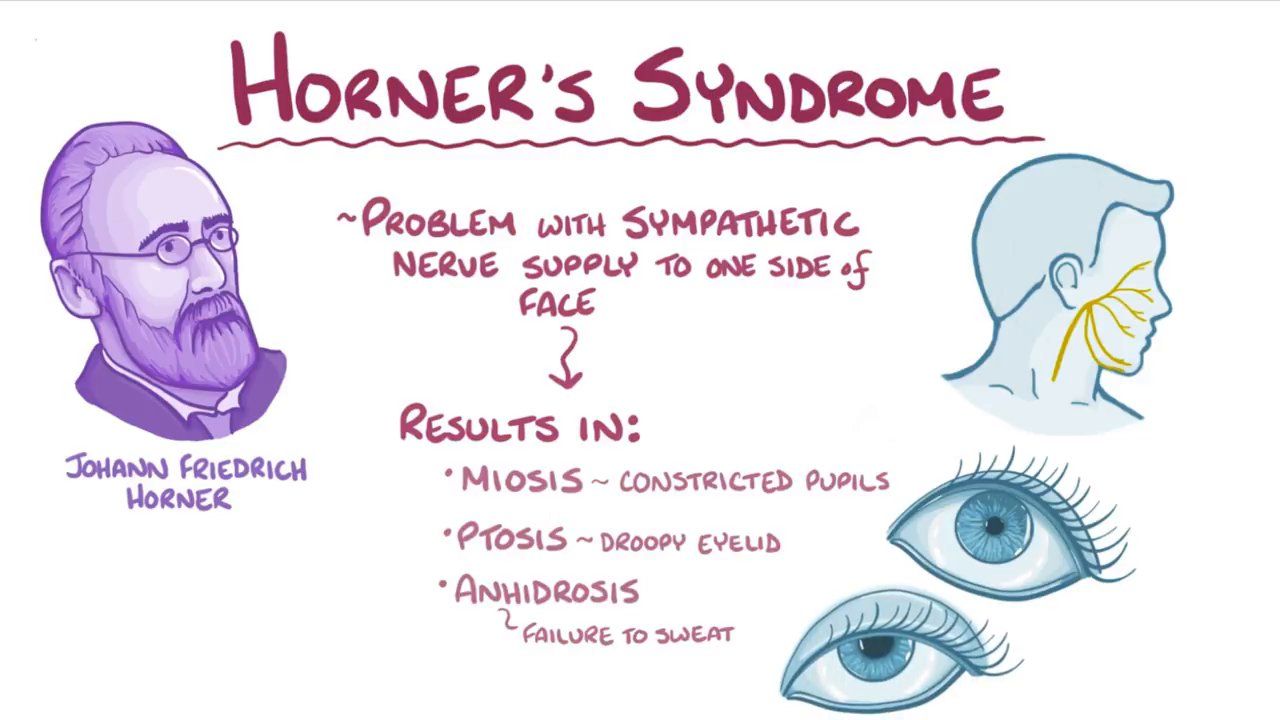
Horner Syndrome is a neurological condition characterized by a disruption in the pathway of sympathetic nerves, resulting in specific symptoms affecting the eye and surrounding facial tissues on one side of the face. Differential diagnosis plays a crucial role in identifying the underlying cause of Horner Syndrome. Physiotherapy professionals should be aware of the red flags associated with this condition and collaborate with other healthcare specialists to ensure timely intervention and optimal management.
The physiotherapy role in the management of Horner Syndrome is essential. Physiotherapists play a crucial role in recognizing the signs and symptoms of Horner Syndrome and referring patients to appropriate specialists for further evaluation and diagnosis. Physiotherapy input can help identify underlying causes of the condition, such as aneurysms or carotid artery dissection, which require specialized consultations with neurosurgery, interventional radiology, or oncology.
Collaboration with specialists is vital for the optimal management of Horner Syndrome. Physiotherapists work alongside pulmonologists, internal medicine physicians, neurologists, and neuro-ophthalmologists to ensure comprehensive care for patients. Timely intervention is crucial in improving patient outcomes and preventing complications associated with Horner Syndrome.
Symptoms and Causes
When considering the symptoms and causes of Horner Syndrome, it is important to understand the specific manifestations that can occur as a result of the disruption in sympathetic nerve pathways. Common symptoms of Horner Syndrome include drooping of the upper eyelid (ptosis), constricted pupil (miosis), decreased sweating or lack of sweating on the affected side of the face (anhidrosis), and redness or flushing of the affected side. Horner Syndrome can be caused by blockage or damage to sympathetic nerves leading to the eyes. Underlying causes can vary widely, from middle ear infection to carotid artery dissection. Three different nerve pathways can be involved in Horner Syndrome: first-order (central), second-order (preganglionic), and third-order (postganglionic). Some cases have no known underlying condition and are referred to as idiopathic.
| Symptoms | Causes |
|---|---|
| Ptosis | Middle ear infection |
| Miosis | Carotid artery dissection |
| Anhidrosis | Tumor |
| Flushing | Nerve damage |
| Idiopathic |
Differentiating conditions and underlying conditions play a crucial role in the diagnosis of Horner Syndrome. Management options depend on the underlying cause and may include surgical intervention for treatable causes and medications for symptom management. Physiotherapy plays a role in recognizing signs of Horner Syndrome and referring patients to appropriate specialists. Prognosis factors depend on the underlying cause and the extent of nerve damage. Prompt and appropriate treatment can help prevent complications and improve patient outcomes. By understanding the symptoms and causes of Horner Syndrome, healthcare professionals can provide optimal care and support for individuals affected by this condition.
Diagnosis and Diagnostic Tests
To diagnose Horner Syndrome and determine the underlying cause, healthcare professionals utilize a combination of physical examinations and specialized diagnostic tests. The physical examination involves assessing the patient’s symptoms, such as drooping of the upper eyelid (ptosis), constricted pupil (miosis), and decreased sweating on the affected side of the face (anhidrosis). A key diagnostic test for Horner Syndrome is the eye drop test, also known as pharmacological testing. This test involves instilling eye drops that contain a sympathomimetic drug, such as cocaine or apraclonidine, into the affected eye. If the pupil dilates significantly after the eye drop is administered, it suggests that the underlying cause of Horner Syndrome is a postganglionic lesion. Additional imaging tests may be ordered to identify any structural abnormalities or tumors that may be causing the syndrome. These tests can include chest X-rays, magnetic resonance imaging (MRI), computed tomography (CT) scans, or ultrasound. Differential diagnosis is essential to differentiate Horner Syndrome from other conditions with similar symptoms. Once a diagnosis is made, treatment approaches will depend on addressing the underlying cause, which may involve surgical intervention, medication, or physical therapy.
Treatment Options
Upon making a diagnosis of Horner Syndrome by assessing the patient’s symptoms and conducting diagnostic tests, the next step is to consider the appropriate treatment options. Treatment of Horner Syndrome focuses on addressing the underlying cause. In some cases, surgical interventions may be necessary if the cause is known and treatable, such as a tumor. Medication management may also be prescribed to manage symptoms or address specific causes. Physical therapy or rehabilitation may be recommended to improve function and address any functional limitations. Regular monitoring and follow-up with healthcare providers is essential to track the progress of treatment and ensure optimal management of the condition. It is important to note that the prognosis of Horner Syndrome depends on the underlying cause and the extent of nerve damage. Prompt and appropriate treatment can help prevent complications and improve patient outcomes. Therefore, a comprehensive and individualized approach to treatment is crucial in managing Horner Syndrome effectively.
Prognosis and Complications
The prognosis of Horner Syndrome depends on the underlying cause and the extent of nerve damage. Prompt treatment and management are crucial for better outcomes. In some cases, Horner Syndrome may resolve on its own. However, complications can arise, including vision problems, facial asymmetry, and functional limitations. Long-term management and monitoring may be necessary for some individuals.
| Prognosis Outcomes | Complications |
|---|---|
| Varies depending on underlying cause | Vision problems |
| Nerve damage extent | Facial asymmetry |
| Prompt treatment and management | Functional limitations |
| Resolution of symptoms in some cases |
It is important to address the underlying cause of Horner Syndrome to prevent complications and improve prognosis. Vision problems can include blurred vision, decreased visual acuity, or changes in pupil size, which may require corrective measures such as glasses or contact lenses. Facial asymmetry can affect the appearance and may require cosmetic interventions. Functional limitations can impact daily activities and may necessitate occupational therapy or assistive devices. Regular monitoring and follow-up with healthcare providers are essential for long-term management and to address any potential complications that may arise.
Anatomy and Pathophysiology
Addressing the underlying cause of Horner Syndrome is essential to understanding its anatomy and pathophysiology. Here are three key aspects to consider:
- Sympathetic innervation: Sympathetic fibers innervate the eye through a 3-neuron arc. First-order central sympathetic fibers originate from the posterolateral hypothalamus and descend uncrossed through the midbrain and pons. They terminate in the intermediolateral cell column of the spinal cord at the level of C8-T2. Second-order preganglionic pupillomotor fibers exit the spinal cord at the level of T1 and enter the cervical sympathetic chain.
- Nerve pathway: Horner Syndrome can develop from lesions at any point along the sympathetic pathway. Commonly, disruptions occur in the preganglionic fibers. Lesions causing postganglionic sympathetic dysfunction are typically located intracranially or intraorbitally.
- Lesion locations and clinical features: Abnormalities found in all patients with Horner Syndrome include mild-to-moderate ptosis and miosis. Impaired flushing and sweating may be present on the affected side, depending on the level of the lesion. Iris heterochromia, or a difference in color between the affected and unaffected iris, can also be observed.
Understanding the anatomy and pathophysiology of Horner Syndrome is crucial for accurate diagnosis and appropriate management of this condition.
Epidemiology and Etiology
Horner Syndrome is a neurological condition characterized by disruptions in sympathetic nerve pathways, leading to specific clinical features such as ptosis, miosis, and impaired sweating on one side of the face. The epidemiology of Horner Syndrome reveals that it has a frequency of approximately 1 per 6,250 population. It can occur at any age and in any ethnicity. Horner Syndrome can be congenital, acquired, or purely hereditary. The underlying pathology of Horner Syndrome involves the interruption of sympathetic fibers, which may occur centrally or peripherally. Common lesions causing Horner Syndrome interfere with preganglionic fibers. Virtually all lesions producing postganglionic sympathetic dysfunction are located intracranially or intraorbitally. It is important to note that preganglionic Horner Syndrome indicates a serious underlying pathology.
In terms of etiology, Horner Syndrome can have various causes. It can result from a wide range of underlying pathologies, including tumors, trauma, vascular disorders, infections, or idiopathic causes. The interruption of sympathetic fibers at different levels along the pathway can lead to the development of Horner Syndrome. Congenital cases of Horner Syndrome can occur due to birth trauma or nerve injury during delivery. Overall, understanding the epidemiology and etiology of Horner Syndrome is crucial for accurate diagnosis and appropriate management of this condition.